Guest blog with future psychodermatologist Erica Aukerman!
Hello! My name’s Erica Aukerman, and I’m a fourth-year medical student at Indiana University School of Medicine. I recently matched into dermatology, and my interest in the field traces back to before medical school. The ability to have a profound impact on a patient’s quality of life drew me to dermatology originally. I also value the innovative nature of the field and the continuity of care. I want to establish longitudinal relationships with my patients and see them improve over time. Growing up with severe eczema, I understand firsthand the psychological toll that skin conditions can take. As a result, I am passionate about addressing the psychosocial impact of skin disease. Throughout medical school, I have collaborated with dermatologists, psychiatrists, and therapists from across the country on projects within the realm of psychodermatology and hope to continue contributing to this niche field in the future.
Can you tell the readers about what it took to get to this point and what it means for you to have matched at IU? What will the next few years of your career look like, and when do you finally get to claim the title of Dr.?
I truly cannot put into words how excited I am to have matched at my home dermatology program, Indiana University. I am so grateful to continue training under my incredible mentors and alongside wonderful colleagues. It took a lot of hard work to get this point, but I’ve truly loved every step of the way. I worked hard to excel academically in medical school, and I devoted most of my time to learning how to best take care of patients as a physician. I spent any extra time I had establishing connections and exploring the field of dermatology. I will officially become a doctor at the conclusion of medical school (this May). I will complete an intern year in general medicine before entering my three years of dermatology residency. At the completion of residency, I will officially be able to call myself a dermatologist.
2. How did you become interested in psychodermatology? Was there a personal component to your interest?
My interest in psychodermatology stems from my personal experience with eczema, but it has been fueled by my interactions with patients who suffer from life-limiting skin conditions. My involvement with Camp Wonder, a camp dedicated to empowering children with severe skin diseases, sparked my interest in the psychosocial impact of skin disease. Spending prolonged periods of time with children who have conditions like epidermolysis bullosa and harlequin ichthyosis opened my eyes to the daily hardships they face. I want to serve as a pillar of support for these patients and their families and learn as much as I possibly can during my training to provide them with the highest level of evidence-based, compassionate care.
3. Can you name one or two of the most fascinating things you have learned about the mind/body/skin connection?
One thing that fascinates me most about the mind/body/skin connection is the intimate link between mental stress and exacerbation of certain skin conditions.
4. What research have you been involved in recently that you would like to share with my followers who are interested in body-focused repetitive behaviors?
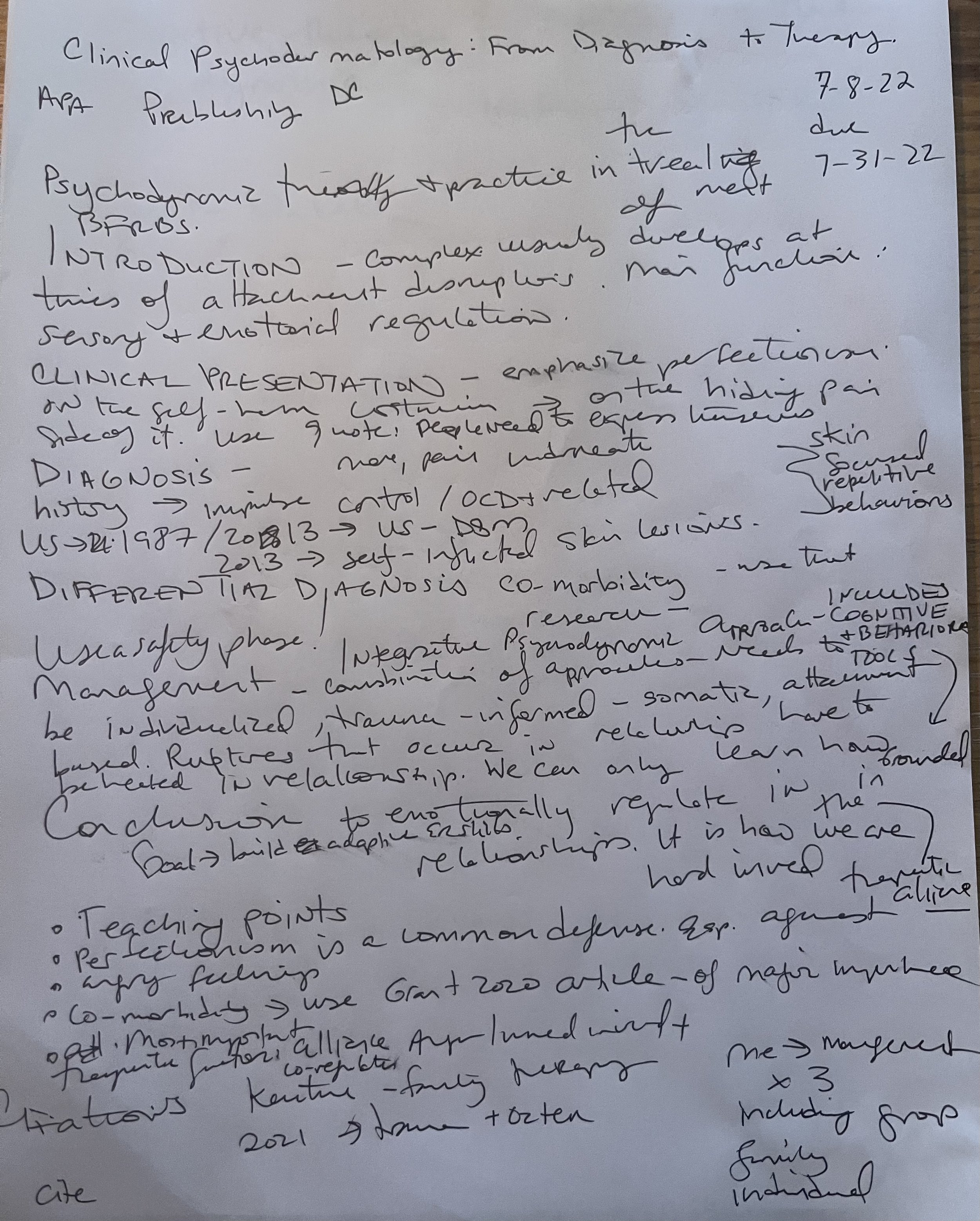
I recently helped Stacy with a write-up focused on the benefits of psychodynamic therapy for patients with body-focused repetitive behavior disorders. We shared the story of a patient with multiple psychiatric comorbidities whose skin-picking disorder responded well to intensive psychodynamic therapy.
5. How do you hope to use your knowledge to advance the field of psychodermatology?
I hope to use my platform to draw more attention to the importance of this field. Skin conditions do not exist in isolation, and it’s important to address the mind/body/skin connection for comprehensive patient care. I want to find more ways to incorporate quality-of-life metrics into dermatologic care and continue researching ways to improve the everyday lives of patients who suffer from dermatologic conditions with strong psychological implications.
6. Can you give a sneak peek of your thoughts about my book for your upcoming book review through Dermatologic Therapy?
It is an easy-to-read book that supports the efficacy of a psychodynamic approach in the treatment of body-focused repetitive behaviors. Stacy does a wonderful job weaving compelling case studies with the practicalities underlying her therapeutic approach. Her patients' treatment responses speak volumes to the work she does and her work warrants expanded use of psychodynamic therapy across the field of psychodermatology. This book not only benefits those who serve patients from a medical or therapeutic standpoint but also offers support and validation to those who personally struggle with body-focused repetitive behaviors.